|
Congestive Heart Failure
Congestive heart failure (CHF)
or simply heart failure, is a condition where
the heart fails to pump adequate blood to meet the body's need.
Unlike a heart attack, the heart does not stop beating - rather,
it weakens over the course of months or years so that it cannot
pump enough blood. As a result, pulmonary congestion
or fluid build up occurs in the lungs.
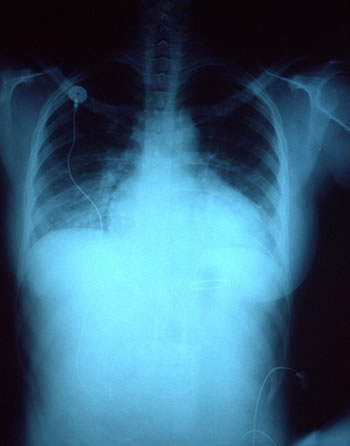
Enlarged heart and accumulation of fluids
in the lungs in congestive heart failure.
There are several ways that the heart can fail:
- Weakened heart muscle
Muscles of the pumping chamber of the heart can become so stretched
and weakened that the heart cannot pump enough blood to reach
all of the body's tissues.
- Loss of elasticity of the heart muscle
The heart muscle can become stiffened or thickened. This prevents
enough blood from filling the pumping chamber, and as a result,
not enough blood is pumped out.
- Abnormal heart valves
Stenosis or narrowing of the heart valves (such as aortic
valve stenosis, mitral
valve stenosis, pulmonary
valve stenosis) and prolapse or floppy valves (such as mitral
valve prolapse) can increase the workload of the heart.
- Heart remodeling
To compensate for inefficient pumping, the heart can undergo
irreversible structural changes called heart remodeling.
In some cases, the left ventricle can enlarge and change shape.
There are changes at the cellular level as well, such as early
cell death that causes the heart muscle cell to die.
There are two types of heart failures:
- Systolic dysfunction or failure
This type of heart failure is the most common type. It occurs
during the systolic or contraction phase, and affects the left
side of the heart. Here, the left ventricle is usually enlarged
and fluid accumulates in the lungs.
- Diastolic dysfunction or failure
This type of failure occurs during the diastolic or relaxtion
phase, and usually affects the right side of the heart. It is
usually caused by thickened heart muscle which prevents the
heart to relax completely. As a result, blood cannot efficiently
enter the heart and backs up in the veins and surrounding heart
tissue.
Symptoms of Heart Failure
The symptoms of congestive heart failure include:
- Fatigue
- Shortness of breath, especially during physical activity or
when lying down
- Wheezing or dry cough, especially when lying down
- Sleep apnea, or disordered or inability to breathe at night
- Loss of appetite and weight loss (loss of muscle mass)
- Swelling of the feet, ankles, and legs
- Swelling or discomfort in the upper abdomen, sometimes enlargement
of the liver
When fluid builds up in the lungs in a condition called pulmonary
edema, the patient may have the following symptoms:
- Cough with pink froth
- Shortness of breath
- Sensation of drowning, or bubbling in the lungs
- Clammy, pale, and bluish-tinged skin.
These symptoms (especially the symptoms of pulmonary edema) are
serious and require immediate medical help.
Diagnosis
Your doctor would perform the following tests to diagnose this
condition:
- Physical examination
Irregular heart sound, such as ventricular gallop or a distinct
hearbeat can be heard using a stethoscope. Rales or crackling
breath can also be heard. Enlarged and tender liver, swollen
feet and legs, fluid retention and elevated pressure on the
neck veins and arteries can also be diagnosed.
- Chest X-Ray and Electrocardiogram
Enlarged heart can be seen using a chest x-ray and electrocardiogram
(ECG). Abnormal heart rhytm can also be visualized with an ECG.
- Echocardiography
Also called Doppler flow test, echocardiography is the best
diagnostic test for congestive heart failure. Here, ultrasound
is used to visualize the beating heart, valve function, and
blood flow. By calculating the ejection fraction or amount of
blood pumped out during a heartbeat, your doctor can determine
the severity of the condition.
- Coronary Angiography
In this test, a catheter is inserted into the heart to measure
internal blood pressure.
Causes of Congestive Heart Failure
Increased workload and stress on the heart caused by the following
conditions can lead to heart failure:
- Heart Attack
Thanks to modern medicine and prompt treatment, heart attack
or myocardial infarction is now very survivable. The attack
itself, however, can lead to dramatic increase in developing
congestive heart failure.
- Coronary Artery Disease or Atherosclerosis
In this condition, the arteries of the heart is blocked by atherosclerotic
plaque deposit.
- High Blood Pressure
In addition to directly causing a heart attack or myocardial
infarction, hypertension or high blood pressure can also cause
heart failure without an attack. High blood pressure causes
the heart muscle to thicken, and over time the increased force
to pump blood can cause it to weaken.
High blood pressure is implicated in over 75% of all cases of
heart failure.
- Heart Valve Abnormalities
Abnormal narrowing or improper closing of the valve leaflets
can interefere with blood flow and cause the heart to work harder.
Left untreated, diseases such as rheumatic fever can cause scarring
of the heart valves. Most heart valve abnormalities, however,
occurs during fetal development and is congenital or present
at birth.
- Cardiomyopathies
These diseases damage the heart muscles and causes them to become
too thin or too thick.
In Idiopathic Dilated Cardiomyopathy, the heart ventricle become
enlarged and the muscles become too thin. Although the cause
is unknown, it is thought that viral infection triggers the
body's own immune system to erroneously attack and kill heart
muscle cells.
In Hypertrophic Cardiomyopathy, it is thought that loss of power
in the heart muscle cells cause the heart to compensate by building
more (and thus thickening) the heart muscle. This rare condition
often made news as the cause of death of young athletes.
Chronic alcohol abuse can also reduce the heart muscle's effectiveness
and cause damage leading to cardiomyopathy.
- Remodeling of the heart
Remodeling is structural and cellular change of the heart in
response to impaired heart functions.
For example, to compensate for increased input due to high blood
pressure, the heart can grow in size or enlarge. This is often
done by elongation of the heart muscle cells, which result in
thinner and weaker cell walls. The cell muscle itself becomes
thinner and weaker.
To compensate for weakened pumping action, the nervous sytem
can signal the heart to beat faster. In the long run, this actually
create more damage.
The body's blood vessel can also change: to compensate for lower
blood flow, they constrict and become more narrow. In turn,
this cause the heart to work harder and beat faster thus increasing
blood pressure and compounding the vicious cycle that will ultimately
lead to heart failure.
- Various Other Diseases
Hyperthyroid disease or other tachycardias
(rapid heart rate) can stress the heart by increasing its workload.
Risk Factors for Congestive Heart Failure
About 5 million people in the United States suffer from this
condition, and every year about 500,000 new cases are reported.
About 250,000 people die every year because of heart failure.
The risk factors of congestive heart failure include:
- Age
Since this disease is a progressive condition (ie. it worsen
with time), the risk of heart failure is increased with age.
It is now the most common reason for hospitalization in the
elderlies.
- Genetics
Tendency to develop heart failure, especially when caused by
cardiomyopathies, may run in families. It is important to note
that dietary habit of the family must be taken into account:
when all members of the family eat high fat, high cholesterol
diet, this maybe the underlying cause of atherosclerosis, not
genetics.
- Gender
Men are at higher risk of developing heart failure than women,
although the difference narrows with advancing age.
- Ethnicity
African Americans are at higher risk than Caucasians, and have
higher mortality rate due to heart failure. Afrian Americans
tend to develop diastolic heart failure (inability of the heart
to relax properly), whereas Caucasians tend to develop systolic
failure (inability to pump blood) first.
- Alcohol Abuse and smoking
Chronic alcohol use can lead to high blood pressure, heart muscle
damage, and even cause cardiomyopathy. The carbon monoxide in
cigarettes is thought to damage the heart muscle and increase
its susceptibility to virus infection.
- Exercise and Dietary Habits
Sedentary lifestyle, lack of exercise and eating fatty foods
can increase the risk of developing coronary artery disease,
which lead to heart failure.
- Presence of Other Diseases
In addition to coronary artery disease, previous heart attack,
high blood pressure, and valve abnormalities, other diseases
such as diabetes, emphysema, HIV-infection and other infection-caused
cardiomyopathies, hyperthyroidism, amyloidosis, and myocarditis
can lead to increased risk of heart failure.
In rare instances, women can also suffer heart failure during
childbirth in a condition called peripartum cardiomyopathy.
- Side Effects of Medications
Older chemotherapy used to treat childhood cancers, use of anabolic
steroids, and certain anti-fungal drugs can lead to heart failure.
- Vitamin Deficiency
Lack of thiamin (vitamin B1) can lead to cardiomyopathy.
Luckily, this condition is reversible by adding enough vitamin
B to the diet.
Congestive Heart Failure Treatment
Treating heart failure almost always mean treating the underlying
cause of this condition. These include lifestyle changes (stop
smoking and stop drinking alcohol) and dietary changes (eat healthier
food, stop eating fatty diets) to treat coronary artery disease,
treating high blood pressure and heart valve abnormalities, and
so forth.
Medicines that improve heart function can also be prescribed:
- Diuretics
Also called water pills, diuretics reduce the volume of blood
and decreases congestion or fluid build ups by inducing the
kidney to release salt. This reduces the blood pressure and
lightens the workload of the heart.
- Angiotensin-Converting Enzyme (ACE) Inhibitors
These medications lower the blood pressure by enlarging or dilating
the arteries and also by reducing the volume of blood.
ACE Inhibitors significantly reduce the death rate associated
with heart failure, and therefore becomes the front-line medications
for this disease.
- Other Vasodilators
For some reason, ACE Inhibitors are less effective in African
Americans. In addition to this medicine, other vasodilators
(medicines that dilate the blood vessels) such as hydralazine
and nitrates are often used.
- Inotropic medications
These drugs strengthen the heart's contraction so it can pump
better. These include digitalis (digoxin), dopamine, and others.
- Beta blockers
In combination with other medications, beta blockers can be
prescribed to slow the heart rhythm. Beta blockers should be
used with caution since they can also decrease the pumping efficiency
of the heart.
Severe heart failure may require surgery, such as baloon dilaton
of artery blockages, heart transplantation, pacemaker implants
to control the heart rhythm, and insertion of portable pumps to
infuse medications. In cases of valve defects, surgery to repair
or replace the damaged valves may be necessary.
Prognosis
The prognosis of heart failure is fair to poor, although advances
in medicine continues to greatly increase expected lifespan. The
annual mortality in people with mild, stable symptoms of heart
disease is about 10%. In those with severe and progressive disease,
the mortality rate can be as high as 50%.
|